Express Scripts’ coverage of Viagra depends heavily on your specific prescription drug plan. Check your formulary–that’s the list of drugs your plan covers–for details. This list is often available online through your plan’s website or member portal.
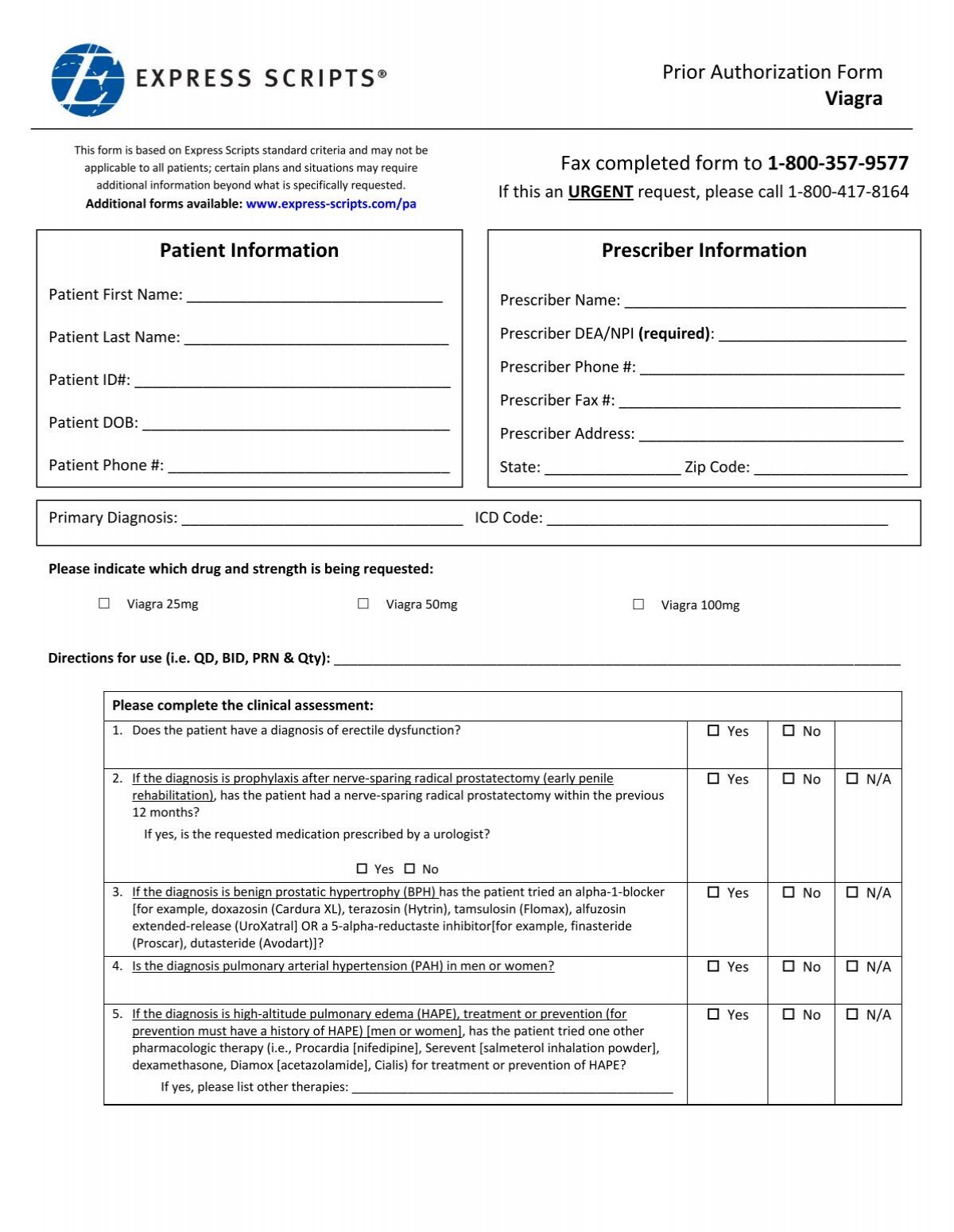
Prior authorization might be required. This means your doctor needs to get pre-approval from Express Scripts before they can prescribe Viagra under your plan. The process involves submitting specific information about your medical condition and prescription needs. Contact your doctor or Express Scripts directly to understand the exact requirements for prior authorization.
Cost sharing varies widely. Even if Viagra is covered, you’ll likely pay a copay or coinsurance. The amount depends on your plan’s tier system (e.g., generic, preferred brand, non-preferred brand) and your individual benefits. Review your Summary of Benefits and Coverage (SBC) for a clear breakdown of expenses. Generic alternatives, if available and covered, could significantly reduce your out-of-pocket costs.
Remember to consult your doctor about alternative treatments if Viagra isn’t covered or is too expensive. They can discuss other options and help you manage your prescription costs.
- Does Express Scripts Cover Viagra?
- Factors Affecting Coverage
- How to Check Coverage
- Alternatives to Viagra
- Disclaimer:
- Express Scripts’ Prescription Drug Coverage: General Overview
- Viagra and its Place in Express Scripts’ Formularies
- Factors Influencing Viagra Coverage: Plan Type and Tier
- Prior Authorization Requirements for Viagra on Express Scripts
- Required Documentation for Prior Authorization
- Appealing a Denied Prior Authorization
- Generic Alternatives and Their Coverage Under Express Scripts
- Finding Affordable Options
- Other Generic PDE5 Inhibitors
- Prior Authorization Process
- Cost-Sharing: Copay, Coinsurance, and Deductibles for Viagra
- Understanding Your Costs
- Finding Your Plan Details
- Finding Accurate Coverage Information: Utilizing Express Scripts Resources
Does Express Scripts Cover Viagra?
Express Scripts’ coverage of Viagra depends entirely on your specific plan. They don’t universally cover it.
Factors Affecting Coverage
- Your insurance plan: The details of your prescription drug coverage are determined by your employer or insurer, not Express Scripts directly. Your plan’s formulary–a list of covered medications–dictates whether Viagra is covered, and at what cost-sharing level (copay, coinsurance).
- Prior authorization: Many plans require prior authorization before covering Viagra. This involves your doctor submitting a request to justify the need for the medication.
- Generic alternatives: Express Scripts, like other pharmacy benefit managers, often prefer generic equivalents. If a generic alternative to Viagra exists and your plan allows substitutions, it will likely be covered more favorably.
How to Check Coverage
- Check your plan’s formulary: Access your plan’s website or contact your insurance provider directly to review the list of covered medications and any cost-sharing details.
- Contact Express Scripts: You can call their customer service line for assistance. Have your member ID ready.
- Talk to your doctor: Discuss alternative medications or options if Viagra is not covered under your plan.
Alternatives to Viagra
If Viagra isn’t covered, your doctor can discuss other treatment options for erectile dysfunction, which may be covered by your insurance.
Disclaimer:
This information is for guidance only and doesn’t constitute medical or insurance advice. Always consult your doctor and insurance provider for accurate and personalized information.
Express Scripts’ Prescription Drug Coverage: General Overview
Check your specific plan’s formulary. This document lists covered medications and their tiers. Tier placement determines your cost-sharing. Generally, lower tiers mean lower out-of-pocket expenses.
Understand your plan’s copay, coinsurance, and deductible. Your responsibility varies based on the medication’s tier and your plan’s design. Higher tiers often require greater cost-sharing.
Prior authorization may be needed for certain medications, including brand-name drugs. Your doctor must obtain approval from Express Scripts before your prescription is filled. This process can add time, so plan accordingly.
Utilize Express Scripts’ online tools. Their website and mobile app provide convenient access to your formulary, benefit information, and prior authorization status. You can also find participating pharmacies nearby.
| Plan Type | Typical Cost-Sharing Features |
|---|---|
| Pharmacy Benefit Manager (PBM) Plan | Varies widely; check your plan’s specific details for copays, deductibles, and coinsurance. |
| Medicare Part D Plan | Features a deductible, initial coverage phase, coverage gap, and catastrophic coverage; details specific to each plan. |
| Commercial Plan | Cost-sharing determined by employer or insurer; check the summary plan description (SPD). |
Contact Express Scripts directly with questions. Their customer service representatives can clarify your coverage, explain the prior authorization process, and help you find the most cost-effective options.
Viagra and its Place in Express Scripts’ Formularies
Express Scripts’ coverage of Viagra, or sildenafil, varies depending on your specific plan and insurance coverage. To determine your coverage, check your formulary. This document lists covered medications and their cost-sharing levels.
Many plans require prior authorization for Viagra. This means your doctor needs to submit a request to Express Scripts before they approve the prescription. Failure to obtain prior authorization often leads to higher out-of-pocket costs. Always confirm your plan’s requirements with your doctor or pharmacist.
Generic sildenafil is often a more affordable option than brand-name Viagra. Express Scripts frequently favors generic drugs due to their lower cost. Discuss the generic alternative with your physician; it’s likely to have similar efficacy.
Express Scripts offers several tools to check drug coverage and costs. Their website and mobile app provide access to your formulary, allowing you to check Viagra’s coverage before filling your prescription.
If you have questions about your specific plan’s coverage, contacting Express Scripts’ customer service directly is the best approach. They can provide the most accurate and up-to-date information regarding your Viagra prescription.
Factors Influencing Viagra Coverage: Plan Type and Tier
Your Viagra coverage depends heavily on your specific health insurance plan and the drug’s tier placement within that plan.
- Plan Type: Medicare Part D plans, for example, often have different formularies (lists of covered drugs) and cost-sharing structures than private insurance plans. Check your specific plan’s formulary to see if Viagra is covered. Medicaid coverage varies by state; some states cover it, while others don’t.
- Tier Placement: Most plans categorize drugs into tiers based on cost and therapeutic value. Viagra is usually in a higher tier (e.g., Tier 3 or Tier 4), meaning higher out-of-pocket costs for you. A lower tier would equate to lower co-pays.
To understand your costs:
- Review your plan’s formulary: This document lists covered medications and their tiers. Your insurance company’s website or member portal will usually provide access.
- Check your Summary of Benefits and Coverage (SBC): This document details your plan’s cost-sharing responsibilities (like copays, coinsurance, and deductibles) for different drug tiers.
- Contact your plan administrator: If you have questions or can’t find the information you need, contact your insurance company directly. They can provide specific details about your coverage for Viagra and potential cost-saving options.
Keep in mind: Generic alternatives to Viagra may be available at lower tiers, reducing your out-of-pocket expenses. Discuss these options with your doctor.
Prior Authorization Requirements for Viagra on Express Scripts
Check your Express Scripts formulary and member handbook for the most up-to-date information. Viagra’s prior authorization (PA) status can vary based on your specific plan. Generally, you’ll need to obtain pre-approval from Express Scripts before receiving coverage. This often involves your doctor submitting a request detailing your medical history and the need for Viagra.
Required Documentation for Prior Authorization
Express Scripts may require specific documentation to approve your request. This commonly includes details about your erectile dysfunction diagnosis, previous treatments, and any relevant health conditions. Your physician should provide this information directly to Express Scripts. Be sure to provide complete and accurate information to facilitate a quick processing of your request. Contact your doctor or Express Scripts customer service for a detailed list of required forms and information.
Appealing a Denied Prior Authorization
If your prior authorization is denied, you can appeal the decision. The appeal process involves providing additional supporting medical documentation that justifies your need for Viagra. Your doctor can assist with this appeal process by gathering further medical evidence and resubmitting the request. Carefully review any denial letter to understand the specific reasons for the denial and ensure you address them in your appeal.
Generic Alternatives and Their Coverage Under Express Scripts
Express Scripts’ coverage of Viagra alternatives depends on your specific plan. Check your formulary for details. Generally, they cover generic sildenafil, the active ingredient in Viagra. This often requires prior authorization.
Finding Affordable Options
Sildenafil is significantly cheaper than brand-name Viagra. Many pharmacies offer generic versions, and Express Scripts often includes these in their formularies at lower cost-sharing levels. However, your out-of-pocket cost will vary based on your plan’s copay and deductible.
Other Generic PDE5 Inhibitors
Express Scripts may also cover other generic phosphodiesterase-5 (PDE5) inhibitors, such as tadalafil (generic Cialis) or vardenafil (generic Levitra). These medications function similarly to sildenafil. Again, formulary status and prior authorization requirements differ based on the specific plan. Contact Express Scripts directly or check your online member portal to confirm coverage.
Prior Authorization Process
Prior authorization is a common requirement for medications like these. This involves your doctor submitting additional information to justify the prescription. The process can add time to obtaining your medication, so plan accordingly. Your doctor’s office can usually manage this process for you.
Cost-Sharing: Copay, Coinsurance, and Deductibles for Viagra
Your out-of-pocket Viagra costs depend on your Express Scripts plan. Check your formulary and Summary of Benefits and Coverage (SBC) for specifics. These documents detail your plan’s cost-sharing structure.
Understanding Your Costs
A copay is a fixed amount you pay each time you fill a prescription. Copays are usually lower than coinsurance amounts. Your Express Scripts plan may require a copay for Viagra, depending on your tier level (generic, preferred brand, non-preferred brand).
Coinsurance is your share of the prescription cost after you meet your deductible. It’s typically expressed as a percentage (e.g., 20%). For example, a 20% coinsurance on a $100 Viagra prescription means you pay $20, and Express Scripts pays $80.
Your deductible is the amount you pay out-of-pocket for covered healthcare services before your insurance kicks in. Once you’ve met your deductible, your coinsurance typically applies to prescription costs.
Important Note: Express Scripts’ coverage, copays, coinsurance, and deductibles vary widely by plan. Contact Express Scripts directly or check your plan documents to determine your exact cost-sharing responsibilities for Viagra.
Finding Your Plan Details
Locate your Express Scripts member ID and access your online account. There, you’ll find your formulary and SBC. Alternatively, contact Express Scripts customer service for personalized assistance. They can help you understand your specific plan benefits and Viagra costs.
Finding Accurate Coverage Information: Utilizing Express Scripts Resources
Check your Express Scripts member portal. Log in using your member ID and password to access your personalized formulary and benefits information. This shows exactly what medications your plan covers, including Viagra, if applicable.
Use the Express Scripts mobile app. Download the app for quick access to your benefits and formulary. The app provides the same information as the online portal but in a convenient mobile format.
Contact Express Scripts customer service. Call their member services line; their representatives can verify coverage for Viagra and answer any questions about your specific plan. Have your member ID ready when you call.
Review your Explanation of Benefits (EOB). After filling a prescription, examine your EOB for details about the amount your plan covered. This confirms your actual out-of-pocket cost for future reference.
Consult your plan documents. Your insurance plan’s booklet contains information about prescription drug coverage, including details on any prior authorizations required for specific medications like Viagra.